UGA receives multiyear grant to address obesity in Georgia

December 5, 2023 by Lauren Baggett in UGA Today
The funds will be used to improve access to healthy foods and physical activity
The University of Georgia has been awarded $804,000 by the Centers for Disease Control and Prevention to improve access to healthy foods and physical activity in Georgia counties with high rates of obesity.
Two decades after being named an epidemic, high rates of obesity persist nationwide. In Georgia, one-third of adults are obese, and therefore, are at higher risk for a number of negative health outcomes – heart disease, stroke, Type 2 diabetes, chronic pain and more.
Eating a healthy diet and getting regular exercise, along with sleep and other health promoting behaviors, is the best way to prevent these chronic diseases, but that’s not always easy to do.
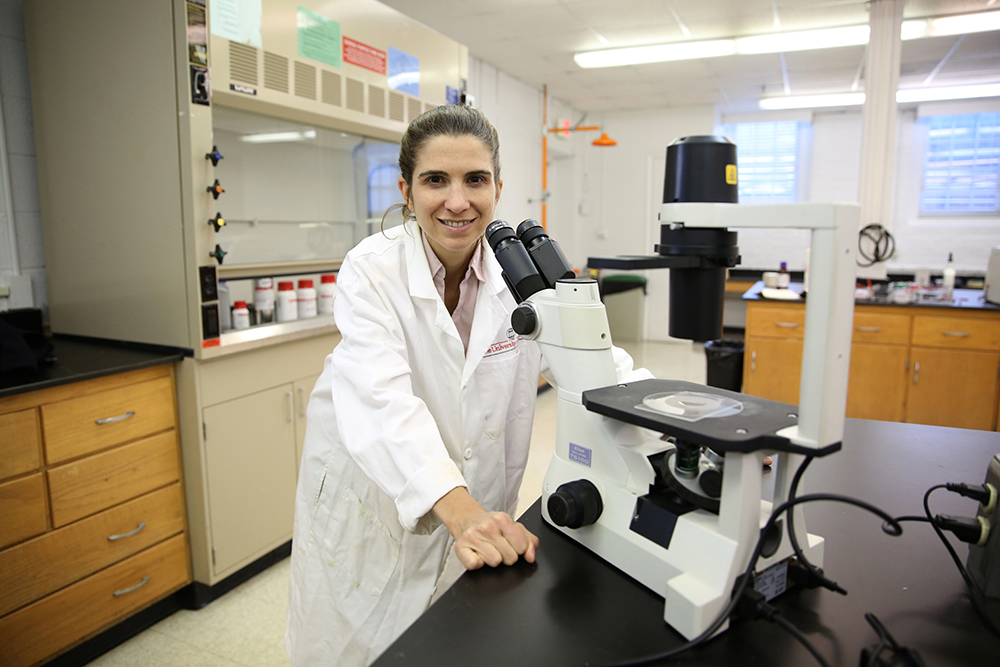
“We can teach people to eat healthy every day, but if those people do not have places to buy affordable fruits, vegetables and whole grains, they will never be able to eat healthy foods that nourish their body. Similarly, we can tell people to exercise and ways they can be active, but if they don’t live in communities where they have safe places to be active, it is not going to happen,” said principal investigator Heather Padilla, an assistant professor of health promotion and behavior in the College of Public Health.
This funding will build on the success of CDC’s High Obesity Program in Georgia, which served Calhoun, Clay, Dooly, Stewart and Taliaferro counties. Together with these communities, UGA research and Extension faculty and staff improved food options for nearly 69,000 people, providing access for 31,041 people to purchase or receive healthier foods in 18 locations and implemented healthy nutrition standards in eight community sites. In addition, all five program communities saw improvements to infrastructure that make it easier to exercise.
Led by an interdisciplinary team of faculty in the UGA College of Public Health, College of Environment and Design, College of Family and Consumer Sciences, College of Agricultural and Environmental Sciences, and UGA Cooperative Extension, this new funding will support UGA Extension and its partners to address obesity in more counties and in new ways.
The project will introduce five new counties – Burke, McDuffie, Sumter, Washington and Rockdale – and will introduce new strategies to create social and physical environments where individuals and families can access healthy foods and places to exercise and play.
“We are expanding from community gardens and retail environments to implementing policies and food service guidelines to ensure healthy foods are available where foods are served and sold, for example, in workplaces or at sports events. We are also working with partners to increase fruit and vegetable voucher incentive programs and produce prescription programs,” said Padilla.
Beginning with Rockdale in the first year, counties will undergo landscape assessments, which will include input from community stakeholders and organizations already working in those communities to align resources and priorities. The new counties will follow the model established in the previous funding cycles, working with county UGA Extension agents who will convene community members from multiple sectors to provide input on community needs and priorities.
“UGA Family and Consumer Sciences Extension agents support people in making healthy decisions and meeting the needs of their families. We bring the latest research-based information and programs to the people in Georgia to improve their lives. This project is a great example of how we are extending the newest science and resources from the university to the citizens of Georgia to address critical community needs,” said Alison Berg, associate professor and Extension nutrition and health specialist in the College of Family and Consumer Sciences.
This new grant will build on previous success and explore opportunities to leverage other Extension and public health programs, resources and relationships, including the UGA SNAP-Ed program.
Making change can be an uphill battle, and having community input and collaboration is essential, noted Padilla and Berg.
“We want to get partners from a variety of domains to the table to try to figure out how we can alter the physical and social environment to at least make it a more level playing field, where people have the opportunity to make the healthy choice,” said Padilla.
Additional project partners include Jung Sun Lee, Georgia Athletic Association Professor in Family and Consumer Sciences in the College of Family and Consumer Sciences, and Donnie Longenecker, a senior lecturer in the College of Environment and Design.